
Polycystic Ovarian Syndrome (PCOS) affects around 1 in 10 women of reproductive age, yet its symptoms and impact vary widely. If you or someone you know has PCOS, you may have experienced challenges like irregular cycles, hormone imbalances, or difficulty managing energy levels. Despite its name, not everyone with PCOS has cysts on their ovaries, making it a complex condition to navigate. The good news? Nutrition can play a key role in managing symptoms and supporting overall well-being.
This is because the diagnosis of PCOS is based on having any two of these three major factors:
- No ovulation causing irregular cycles or a complete lack of periods
- Excess male hormone production (e.g. testosterone) which can be detected through blood tests
- Cysts on the ovaries as detected via an ultrasound
The cause/s of PCOS is still not fully understood, but certain genetics do play a role. PCOS was originally thought to be a fertility issue, however it is now known to be much more complex and associated with several other symptoms:
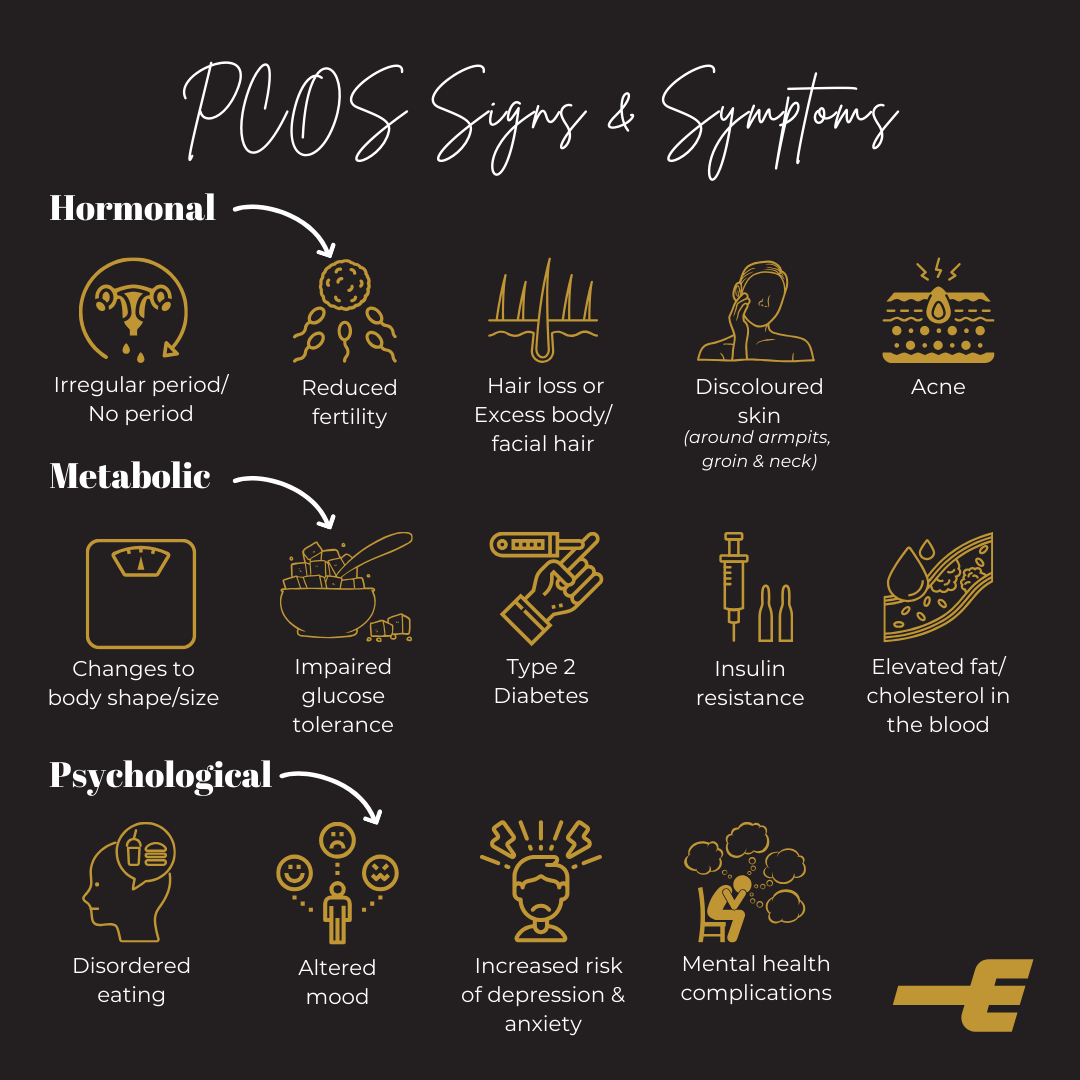
If left undiagnosed, PCOS can lead to a range of long-term health consequences including obesity, high blood pressure, heart disease, diabetes, cancers, infertility, irregular bleeding and mental health disorders.
Unfortunately, there is currently no cure for PCOS. Management instead focuses on treating or reducing the severity of symptoms.
While it’s important to be aware of the symptoms and possible health risks, it’s just as important to note that not everyone with PCOS will experience every symptom and with the same severity. The symptoms and their severity can vary not only between the individual, but also change at different ages.
However, adaptations to nutrition, exercise and lifestyle can help reduce symptoms.
Nutrition Strategies
1. Obtain a strong Nutrition Foundation
Regularly consume a wide variety of fruits & vegetables, lean meats, quality grains, legumes, dairy products and healthy fats as part of your daily intake. Also choosing foods lower in glycaemic index (GI) and having adequate amounts of protein have been found to help manage insulin resistance.
Although, you may have heard all of this before, studies have found that women with PCOS tend to consume diets that are high in fat and too low in fibre and other important nutrients. Eating a healthy, balanced diet is such an important first step.
2. Weight Management
First of all know that PCOS isn’t caused by weight (and not all people with PCOS are overweight!). However striving for continual health improvements, that may lead to weight change in some, can help manage many of the symptoms and risk factors associated with PCOS.
3. Meal Quality
PCOS is related closely to insulin resistance and therefore shares many of the same recommendations associated with diabetes. Therefore women with PCOS may benefit from aiming for lower carbohydrate load at meals and snacks (higher focus on a range of veggies/salad, quality protein and healthy fats) and focusing on simply eating ‘real food’ that is minimally processed.
4. Consider Meal Timing
There is emerging evidence to suggest that meal timing may have an impact on improving insulin sensitivity and hormone production. A recent study found some promising hormonal and metabolic impacts when women with PCOS ate a greater proportion of their food during the first half of the day rather than the latter part of the day. This method is called “front-ending your calories” and could be an easy strategy to try.
5. Supplements to Consider
Supplements are like the ‘icing on the cake’. You need to have a strong nutrition foundation (the cake) before deciding on which ‘sprinkles’ you want over the top. While there are several supplements that may be beneficial in the management of PCOS, evidence is currently very limited. Check out part two for a full breakdown!
Need More Support?
Managing PCOS can feel overwhelming, especially when symptoms vary so much from person to person. Understanding how nutrition fits into your overall approach can help you feel more in control of your health and energy levels. If you’re unsure where to start, our Wellbeing Profile can help identify key areas to focus on. By assessing your current habits and needs, it provides a personalised starting point to work towards feeling and performing at your best.


